Dutch BICAT study proves safety and effectiveness of immediate sequential bilateral cataract surgery
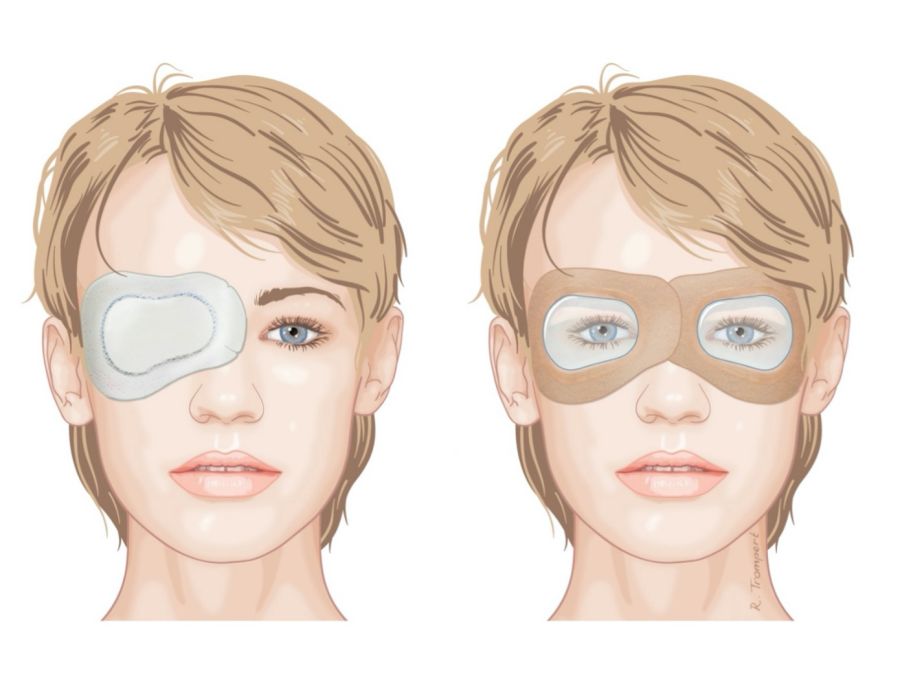
Image caption: “in ISBCS, transparant eye patches are used (right picture) instead of a non-transparant eye patch in DSBCS (left picture)”
News from our full member: University Eye Clinic Maastricht, the Netherlands
Immediate sequential bilateral cataract surgery (ISBCS) offers comparable safety and efficacy to delayed sequential bilateral cataract surgery (DSBCS), according to a major Dutch study. The multicentre randomised controlled trial ‘bilateral cataract surgery in the Netherlands’ (BICAT-NL) was carried out at 10 hospitals in the Netherlands, with 865 patients randomised for either ISBCS or DSBCS, and was coordinated by Rudy Nuijts, Lindsay Spekreijse and Frank van den Biggelaar of the University Eye Clinic Maastricht, the Netherlands.
The primary outcome of the study was to evaluate whether ISBCS is non-inferior to DSBCS with regard to effectiveness, with effectiveness defined as the proportion of patients with a postoperative refraction within 1.0D of target refraction. Secondary objectives included the proportion of patients with a postoperative refraction within 0.5D of target refraction, postoperative visual acuity, patient satisfaction using patient-reported outcome measures (PROMs), incidence of complications and cost-effectiveness.
The guidelines followed for surgery were in line with the ISBCS General Principles for Excellence, with strict separation of procedure, instruments and intraocular medication for right and left eyes.
Turning to the results, the percentage of eyes within 1.0D of target refraction was around 97% for both groups. Similarly, there was no statistical difference regarding percentages of eyes within 0.5D of target in both groups. The uncorrected and best-corrected visual acuity outcomes were also similar between the two groups.
In terms of adverse events, there were no cases of endophthalmitis, one case of bilateral corneal decompensation (DSBCS patient) which developed six weeks after surgery, one case of bilateral uveitis (ISBCS patient) which developed at 10.5 weeks after surgery and one case of bilateral macular oedema (DSBCS patient), which developed at 4.5 weeks after surgery. There were also comparable mild adverse events for ISBCS versus DSBCS such as dry eye and dysphotopsias.
Costs were also less for ISBCS, with a difference of around 403 euros per procedure coming from reduced day admission costs, visits to ophthalmologists and eye drops. Quality of life and patient satisfaction were comparable between the two groups.
The outcomes of the study reflect the growing interest in ISBCS at a time of shrinking healthcare budgets and increased demographic pressure on practitioners to deliver quality eyecare as efficiently as possible. However, there are some potential implementation hurdles, like adapting the logistics at industry partners and hospitals to comply with the safety guidelines, reimbursement issues for surgeons, and training young ophthalmologists to perform the procedures. These hurdles may delay a fast implementation of ISBCS in daily clinical practice.
“in ISBCS, transparant eye patches are used (right picture) instead of a non-transparant eye patch in DSBCS (left picture)”